The Centers for Medicare and Medicaid Services (CMS), which administers Medicare, has developed a host of resources over the years to combat fraud and safeguard the integrity of Medicare, including a nationwide network of Unified Program Integrity Contractors (UPIC).
UPIC audits are not randomly assigned to test compliance; rather, they are focused and targeted investigations intended to collect evidence and documentation of suspected irregularities. CMS will instigate a UPIC audit only when the agency suspects fraud, waste, or abuse at a healthcare or medical facility.
A UPIC auditor may request medical records, conduct patient and employee interviews, make in-person site visits, analyze data and error rates, and refer cases of suspected Medicare fraud to the Office of Inspector General (OIG). Dealing with this type of audit requires experienced legal counsel, as it is often seen as dealing with the highest level of scrutiny.
What Happens in the UPIC Audit Appeals Process?
Once a claim has been denied following an audit, or worse yet, your practice is accused of Medicare fraud, you have the right to appeal the decision and challenge the audit findings. There are five stages of appeal for unfavorable audit determinations. Some providers are successful within the first stage, but oftentimes, providers will need to go through multiple steps to achieve the desired resolution.
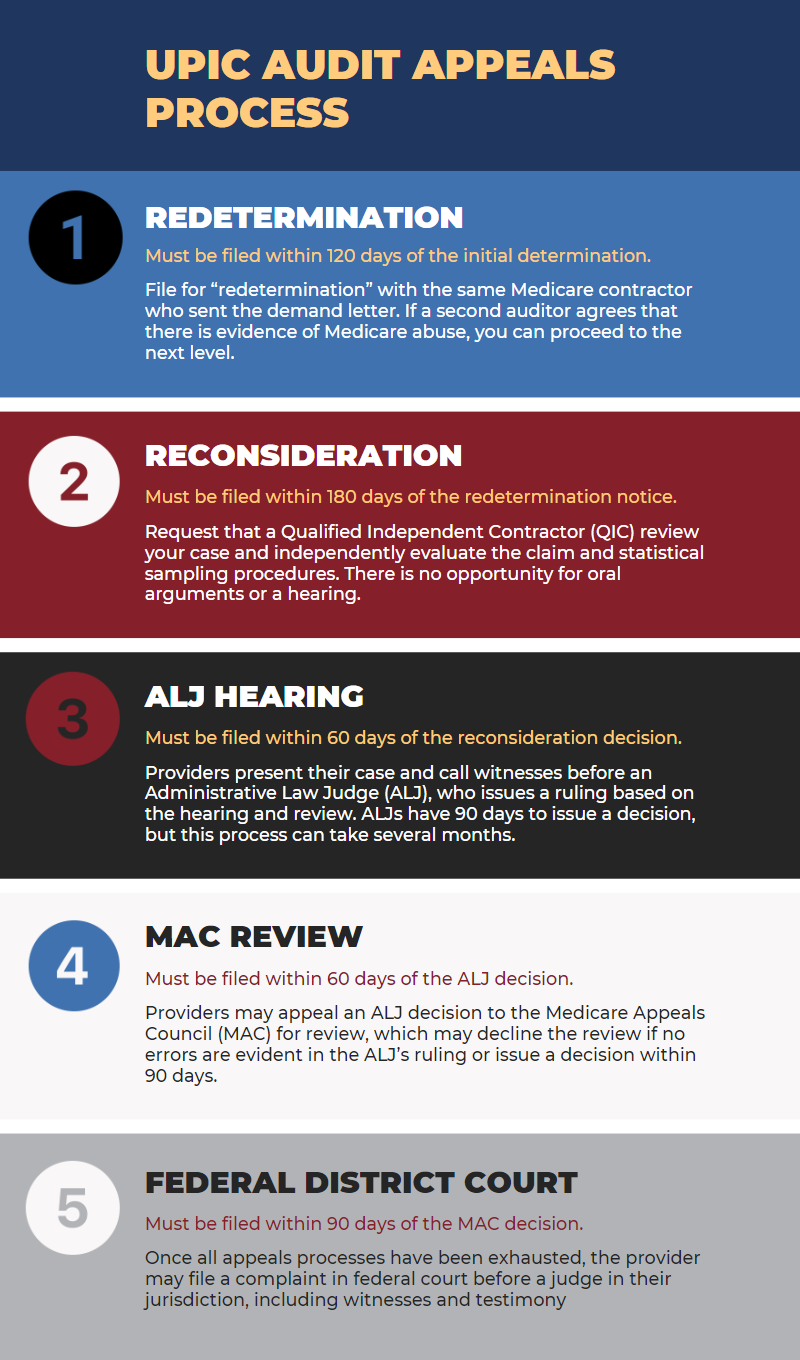
The UPIC audit appeals process is the same as Medicare's Recovery Audit Contractor (RAC) appeals process and follows these five steps:
- Redetermination: Upon receiving an unfavorable UPIC audit determination, the first step is to file for “redetermination” with the Medicare administrative contractor (MAC) who sent the demand letter. This request must be filed within 120 days of the initial determination and include evidence. If a second auditor agrees that there is evidence of Medicare abuse, you can then file at the next level.
- Reconsideration: The second step is to request a Qualified Independent Contractor (QIC) to review your case, who will independently evaluate the claim and statistical sampling procedures. There is no opportunity for oral arguments or hearing. It must be filed within 180 days of the redetermination notice.
- Administrative Law Judge (ALJ) Hearing: As one of the most critical stages, providers can explain their case and call witnesses before an ALJ, who issues their ruling based on the hearing and review. ALJs have 90 days to issue a decision, but this process can take several months. It must be filed within 60 days of the reconsideration decision.
- Medicare Appeals Council (MAC) Review: Providers may appeal an ALJ decision to the MAC for review, which may decline the review if no errors are evident in the ALJ’s ruling or issue a decision within 90 days. It must be filed within 60 days of the ALJ decision.
- Federal District Court: Finally, once all appeals processes have been exhausted, the provider may file a complaint with the federal court before a judge in their jurisdiction, including witnesses and testimony. It must be filed within 90 days of the MAC decision.
Fighting UPIC findings is challenging at any stage of the appeals process, and it can be just as overwhelming as the audit itself, but it can be handled effectively with an experienced healthcare law attorney.
Hendershot Cowart P.C.: Proven Healthcare Law Attorneys
Audits put healthcare providers at risk of expenditures, lost time, and more significant implications. It is important to take proactive steps and conduct internal audits and reviews of medical records. You should also focus on ongoing education to help your staff avoid billing mistakes. As a leader in healthcare law, Hendershot Cowart P.C. can assist you with implementing best practices and developing compliance plans to minimize the chance of an audit. Furthermore, our team has extensive experience defending clients against fraud accusations.
If you are in the midst of a UPIC audit or appeal, please contact the healthcare law team at Hendershot Cowart P.C. to learn more about how we can help. Schedule a consultation by calling today.



